Fighting Lymphoma: Treatment Options Include Alternatives to Chemotherapy
by Jus' Onco | Jul 23, 2025 | Blogs
Lymphoma is a type of cancer that originates in the lymphatic system, a vital component of the body’s immune system. It primarily affects the lymphocytes, a type of white blood cell that plays a central role in protecting the body against infections. Lymphoma is typically divided into two main types: Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL), with NHL being the more common of the two.
Traditional treatment for lymphoma has largely focused on chemotherapy, which involves using drugs to kill or slow the growth of cancerous cells. However, chemotherapy comes with significant side effects that can be challenging for patients. As a result, there is growing interest in exploring alternative treatments and complementary therapies for lymphoma. These treatments aim to reduce the side effects of chemotherapy or, in some cases, offer effective alternatives for patients who are not candidates for chemotherapy.
This article delves into the various treatment options for lymphoma, focusing on those that can serve as alternatives to chemotherapy. These options include targeted therapy, immunotherapy, radiation therapy, stem cell transplants, and integrative therapies, among others. Let’s explore these alternatives in more detail.
Chemotherapy and Its Limitations in Lymphoma Treatment
Chemotherapy has been the cornerstone of lymphoma treatment for many years. It involves the use of powerful drugs that target and kill rapidly dividing cells, including cancer cells. While chemotherapy can be very effective in treating lymphoma, it also affects healthy cells, leading to several side effects. These side effects can range from mild to severe and include nausea, fatigue, hair loss, weakened immune system, and an increased risk of infections.
In addition to these immediate side effects, chemotherapy can sometimes lead to long-term health problems, including infertility, nerve damage, and an increased risk of developing other cancers later in life. As a result, patients and oncologists are increasingly looking for alternative therapies that can provide effective treatment with fewer side effects.
1. Targeted Therapy
Targeted therapy is a treatment that focuses on specific molecules or genes involved in the growth and survival of cancer cells. Unlike chemotherapy, which indiscriminately targets all rapidly dividing cells, targeted therapies are designed to attack only the cancerous cells, thereby minimizing damage to healthy tissues.
There are several types of targeted therapy used in lymphoma treatment:
- Monoclonal Antibodies: These are laboratory-made molecules that can bind to specific antigens on the surface of cancer cells. An example of a monoclonal antibody used for lymphoma treatment is rituximab (Rituxan). Rituximab targets the CD20 protein, which is found on the surface of B lymphocytes, the type of cell that is often involved in non-Hodgkin lymphoma. By targeting this protein, rituximab can help the immune system attack the cancer cells.
- Small Molecule Inhibitors: These drugs work by targeting specific enzymes or proteins that are critical for the survival and proliferation of cancer cells. An example is ibrutinib, which targets the Bruton’s tyrosine kinase (BTK) enzyme involved in B-cell signaling. Ibrutinib has shown promise in treating mantle cell lymphoma and other B-cell lymphomas.
- Gene Editing: Newer forms of targeted therapy, such as CRISPR gene editing, hold potential in modifying the genetic material of cancer cells to disable their ability to grow and spread.
Targeted therapies are often used in combination with other treatments like chemotherapy or radiation therapy, but in some cases, they may be sufficient on their own for patients with certain types of lymphoma.
2. Immunotherapy
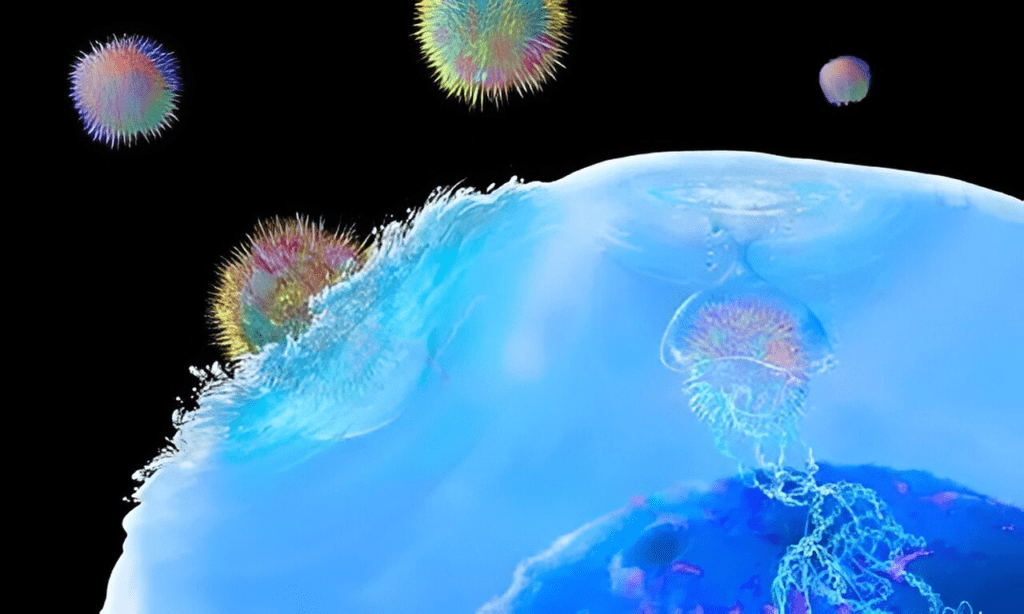
Immunotherapy is a treatment that harnesses the body’s immune system to fight cancer. Unlike chemotherapy, which directly targets cancer cells, immunotherapy works by stimulating or enhancing the immune system’s natural ability to recognize and destroy cancer cells.
There are several types of immunotherapy that can be used to treat lymphoma:
- Checkpoint Inhibitors: These drugs block the checkpoint proteins that prevent immune cells from attacking cancer cells. A notable checkpoint inhibitor used in lymphoma treatment is nivolumab (Opdivo), which targets the PD-1 protein on T-cells, allowing the immune system to attack cancer cells more effectively. Pembrolizumab (Keytruda) is another checkpoint inhibitor used in certain lymphomas.
- CAR-T Cell Therapy: Chimeric Antigen Receptor T-cell (CAR-T) therapy is an innovative immunotherapy that involves modifying a patient’s own T-cells to better recognize and target cancer cells. CAR-T cells are collected from the patient’s blood, modified in the lab to recognize a specific protein on the cancer cells, and then infused back into the patient’s bloodstream. This therapy has been particularly effective for patients with relapsed or refractory lymphoma.
- Cytokine Therapy: Cytokines are proteins that help regulate the immune system. Certain cytokines, such as interleukins and interferons, can be used to enhance the immune response and help the body fight lymphoma. While this form of immunotherapy is still in the experimental stage, it has shown promise in clinical trials.
Immunotherapy offers a less toxic alternative to chemotherapy, with the potential for long-lasting remission. However, it is not suitable for all types of lymphoma, and the side effects, although less severe than those of chemotherapy, can still include fatigue, flu-like symptoms, and, in rare cases, autoimmune reactions.
Looking for affordable cancer care?
At Jus’ Onco Clinic, we offer expert treatment options tailored to your needs, ensuring compassionate care at every step.
3. Radiation Therapy
Radiation therapy uses high-energy radiation to kill cancer cells or shrink tumors. While radiation therapy is often used in conjunction with chemotherapy, it can also be an effective standalone treatment for certain cases of lymphoma, particularly when the cancer is localized in one area of the body.
For early-stage Hodgkin lymphoma, radiation therapy may be used alone or in combination with chemotherapy. In non-Hodgkin lymphoma, radiation can be used to treat localized tumors or to alleviate symptoms like pain or swelling caused by enlarged lymph nodes.
One advantage of radiation therapy over chemotherapy is that it can target specific areas of the body, which minimizes the risk of damage to healthy tissue. However, radiation also carries its own risks, such as skin irritation, fatigue, and an increased risk of secondary cancers in the treated area.
4. Stem Cell Transplants
Stem cell transplants are used for patients whose lymphoma has relapsed or is resistant to other treatments. There are two main types of stem cell transplants:
- Autologous Stem Cell Transplant: In this procedure, a patient’s own stem cells are collected before they undergo high-dose chemotherapy or radiation. After the chemotherapy or radiation, the stem cells are reinfused into the patient to help the bone marrow recover and produce new blood cells.
- Allogeneic Stem Cell Transplant: This involves using stem cells from a donor. It is typically used for patients with high-risk lymphoma. Allogeneic transplants have the potential to provide a more powerful immune response against the cancer but carry a higher risk of complications, such as graft-versus-host disease.
Stem cell transplants are highly effective for certain types of lymphoma, but they come with significant risks, including infections, organ damage, and graft-versus-host disease.
5. Integrative and Complementary Therapies
In addition to the conventional treatments for lymphoma, many patients turn to integrative therapies to complement their medical treatment and improve their quality of life. These therapies include:
- Acupuncture: Acupuncture can help manage pain, reduce nausea, and alleviate some of the side effects of chemotherapy and radiation therapy.
- Herbal Supplements: Some patients use herbs to boost the immune system, reduce inflammation, or manage symptoms such as nausea and fatigue. However, it is important to consult with a healthcare provider before using herbal supplements, as they can interact with conventional treatments.
- Mind-Body Techniques: Techniques such as yoga, meditation, and mindfulness can help manage stress, improve emotional well-being, and enhance the body’s ability to cope with cancer treatment.
While integrative therapies are not a substitute for conventional treatments, they can offer valuable support in managing symptoms and improving overall quality of life.
Conclusion
Lymphoma treatment has traditionally relied on chemotherapy, but with advancements in medical research, there are now several alternatives that can be used alone or in combination with other therapies. Targeted therapies, immunotherapy, radiation therapy, stem cell transplants, and integrative therapies offer patients with lymphoma a range of options that can be tailored to their specific needs. These treatments not only provide hope for patients who are unable to tolerate chemotherapy but also have the potential to improve survival rates and reduce the side effects associated with traditional cancer therapies.
Ultimately, the best treatment approach for lymphoma will depend on the type and stage of the cancer, as well as the individual patient’s health status and preferences. It is essential for patients to discuss their treatment options with their healthcare providers to develop a comprehensive plan that works best for them. As research into lymphoma treatment continues to evolve, the future looks promising for more targeted and less toxic therapies that can help more patients achieve long-term remission and a better quality of life.
Looking for affordable cancer care?
At Jus’ Onco Clinic, we offer expert treatment options tailored to your needs, ensuring compassionate care at every step.
Frequently asked Questions
1. Are there alternatives to chemotherapy for lymphoma treatment?
Yes. Several effective alternatives to chemotherapy include targeted therapy, immunotherapy, radiation therapy, and stem cell transplants. These treatments can be used alone or in combination based on the lymphoma type and stage.
2. What is the role of immunotherapy in treating lymphoma?
Immunotherapy boosts the body’s immune system to fight cancer. Options like CAR-T cell therapy and checkpoint inhibitors (e.g., nivolumab, pembrolizumab) have shown strong results, especially for relapsed or refractory lymphomas.
3. Can radiation therapy replace chemotherapy in lymphoma treatment?
In early-stage or localized lymphoma, radiation therapy can be used as a standalone treatment or with limited chemotherapy. It offers targeted tumor control with fewer systemic side effects than full chemotherapy.
4. What is targeted therapy, and how does it work for lymphoma?
Targeted therapy attacks specific proteins or pathways cancer cells rely on, minimizing harm to healthy cells. Drugs like rituximab (monoclonal antibody) and ibrutinib (BTK inhibitor) are commonly used in non-Hodgkin lymphoma.
5. Are there holistic or integrative approaches that help lymphoma patients?
Yes. Complementary therapies like acupuncture, yoga, herbal support (with medical advice), and mindfulness can ease symptoms, reduce treatment side effects, and improve emotional well-being alongside conventional care.


