Understanding Targeted Therapy Drugs: The Next Step in Personalized Cancer Treatment
by jusonco.com | Aug 16, 2025 | Blogs
Introduction
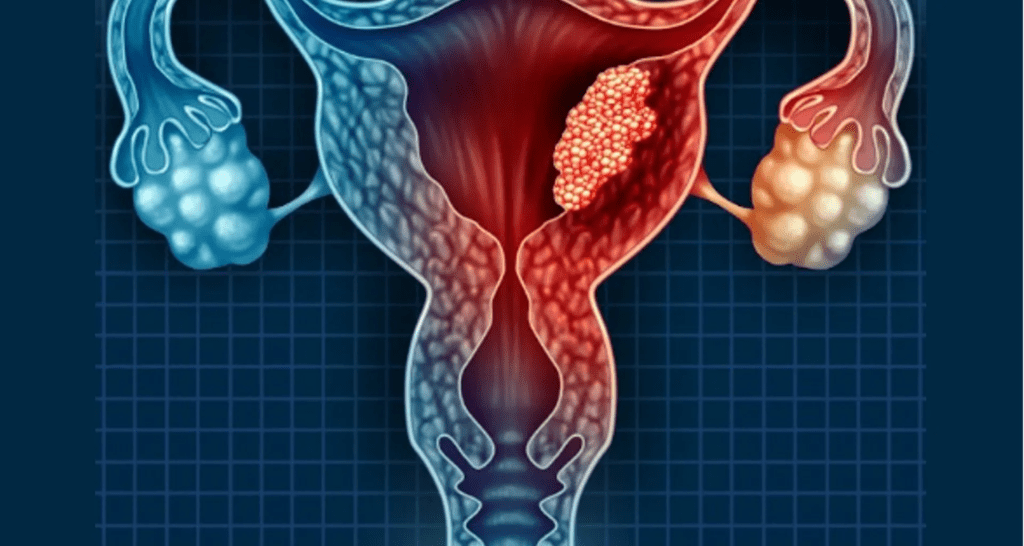
In the fight against cancer, treatments have evolved far beyond one-size-fits-all approaches. Targeted therapy drugs represent a breakthrough, focusing on the specific genetic changes that drive cancer growth. Unlike traditional chemotherapy, these drugs aim to attack cancer cells while minimizing damage to healthy tissues. This approach is particularly promising for patients seeking more effective results with fewer side effects.
In this article, we’ll explore the mechanisms, benefits, and examples of targeted therapy drugs that are transforming cancer care.
Get Affordable Targeted Therapy in Chennai from Jus’Onco Clinic
What is Targeted Therapy?
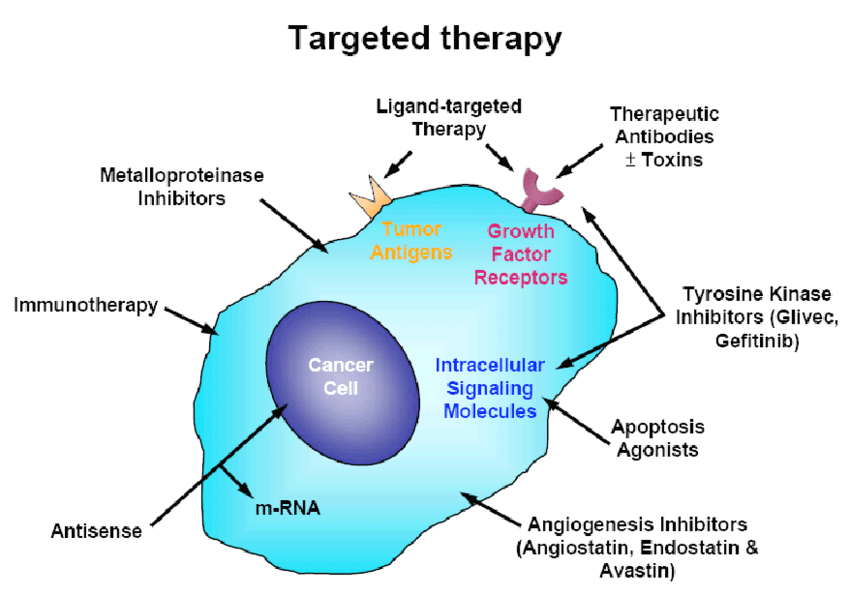
Targeted therapy is a form of precision medicine designed to attack cancer cells by focusing on specific molecular targets involved in cancer cell growth and survival. By honing in on these targets, the treatment spares healthy cells, reducing collateral damage.
How it Differs from Chemotherapy
While chemotherapy works by killing all rapidly dividing cells (both healthy and cancerous), targeted therapy drugs are more selective. This precision leads to fewer side effects and can be more effective for certain cancer types.
Types of Targeted Therapy Drugs
- Monoclonal Antibodies – Laboratory-produced molecules that bind to specific antigens on cancer cells.
- Small Molecule Inhibitors – Drugs that block specific enzymes or proteins essential for cancer cell growth.
- Angiogenesis Inhibitors – Prevent the formation of new blood vessels that feed tumors.
Common Examples in Use
- Trastuzumab (Herceptin) – Used for HER2-positive breast cancer.
- Imatinib (Gleevec) – Effective against chronic myeloid leukemia (CML).
- Bevacizumab (Avastin) – Blocks angiogenesis in various cancer types.
When is Targeted Therapy Used?
Doctors may recommend targeted therapy when:
- Genetic testing reveals specific mutations.
- Standard treatments have failed.
- Cancer is aggressive and needs a more focused approach.
Advantages of Targeted Therapy
- Greater treatment precision.
- Reduced systemic toxicity.
- Potential for combination with other treatments.
Conclusion
Targeted therapy drugs are reshaping cancer care by offering a more precise, less invasive alternative to traditional treatments. However, they aren’t suitable for every patient—success depends on genetic testing and the cancer’s unique profile. By consulting with oncology specialists and exploring personalized treatment options, patients can make informed decisions for better outcomes.
1. How do doctors decide if I need targeted therapy?
Doctors perform molecular or genetic testing on your cancer cells to check for specific mutations or proteins that targeted drugs can act on.
2. Are targeted therapy drugs safe?
They generally cause fewer side effects than chemotherapy, but can still lead to issues like skin rash, fatigue, or high blood pressure depending on the drug.
3. Can targeted therapy replace chemotherapy?
In some cancers, yes. But often, targeted therapy is used alongside chemotherapy, immunotherapy, or radiation for better results.
4. Is targeted therapy available in Chennai?
Yes. Clinics like Jus’Onco in Chennai offer affordable targeted therapy options after confirming eligibility through diagnostic testing.
5. How long will I need to take targeted therapy?
Treatment duration varies based on the type of cancer, stage, and how well your body responds. It could be a few months to several years.